Since the escalation of the war in Ukraine in February 2022, the number of people with serious and severe injuries requiring complex care has increased dramatically. This includes people with blast injuries, shrapnel wounds and amputations, all of whom require intensive, specialised care. According to the Ministry of Social Policy of Ukraine, since the escalation, around 300,000 people have been registered as living with physical disabilities. The increased demand for early rehabilitation services has put an additional strain on the country’s healthcare system. In response, Médecins Sans Frontières launched an early rehabilitation project at Cherkasy Hospital in central Ukraine in March 2023. The project combines physical therapy, psychological support and care for patients with special needs that war-wounded people face in the early stages of recovery.
“All injuries take time” – this sentiment resonates deeply with both the medical staff and patients of Cherkasy Hospital, and it has a special meaning for each group. For physical therapists, it means the importance of every minute spent on procedures and exercises immediately after surgery. For psychologists, it means the value of timely counselling sessions and emotional support. For patients, it is a reminder that the healing process, both physical and emotional, is a journey that takes time and perseverance.





Read also: Deputy Chief Coordinator of Médecins Sans Frontières in Ukraine Andriy Slavutskyi: Our task is to support access to decent medicine
Ihor’s story
For over a month now, 27-year-old Igor has been undergoing treatment for numerous injuries he sustained during a shelling in Sumy Oblast. These include small fragments of shrapnel in his eyes and a broken wrist. “At night, the pain is unbearable,” says Igor. “I screamed in pain and even asked to have my arm amputated.”
Oleksiy Taranenko, a physical therapist with Doctors Without Borders, uses therapeutic exercises and electrotherapy to treat Ihor’s injured arm, and the patient’s condition is slowly improving. “Last night I slept through the night for the first time in a week,” says Ihor. Over the past weeks, he has regained some mobility and can now hold a litre bottle of water for short periods of time.
“Those few moments when he could hold something without sharp pain, with a sense of confidence, were a real achievement, and we celebrated it,” Taranenko says. “We show patients that their condition can improve; it’s a powerful incentive for recovery.”





Read also: HEST courses: preparing healthcare professionals to work in extreme conditions
The number of patients is growing
Many of the injuries treated at the Cherkasy hospital are related to the explosions, and the number of patients with amputations is growing. “Patients come in with severe leg injuries because some have stepped on landmines, and some have shrapnel injuries,” says Blanche Daile, physiotherapy manager at Médecins Sans Frontières. “The war has created an ‘epidemic of physical injuries’.
When patients arrive at Médecins Sans Frontières’ (MSF) early rehabilitation unit, they have most likely already been treated in two or three hospitals. In addition to the patients’ primary injuries, Médecins Sans Frontières staff often encounter complications such as muscle atrophy and joint stiffness. This is due to the fact that surgeons often prioritise tissue integrity and wound healing, which diverts attention from restoring limb functionality, despite the fact that this is what is needed for effective rehabilitation.
“Imagine caring for patients who have undergone 20, 30 or even 40 surgeries in a short period of time,” says Vitaliy Pavliyev, head of mental health at Médecins Sans Frontières. “These patients need support from nurses and psychologists. One patient was being prepared for leg amputation, which surgeons could not avoid. Our psychologists worked with him to help him accept the procedure. After the operation, we turned our attention to managing phantom pain.”
Sleep disorders, panic attacks and pain syndromes – especially phantom pain after amputation – are common among Médecins Sans Frontières patients.




Read also: USAID DOBRE program announces recruitment for the training course on “Resilience in public administration: Preparing for the restoration of local communities”
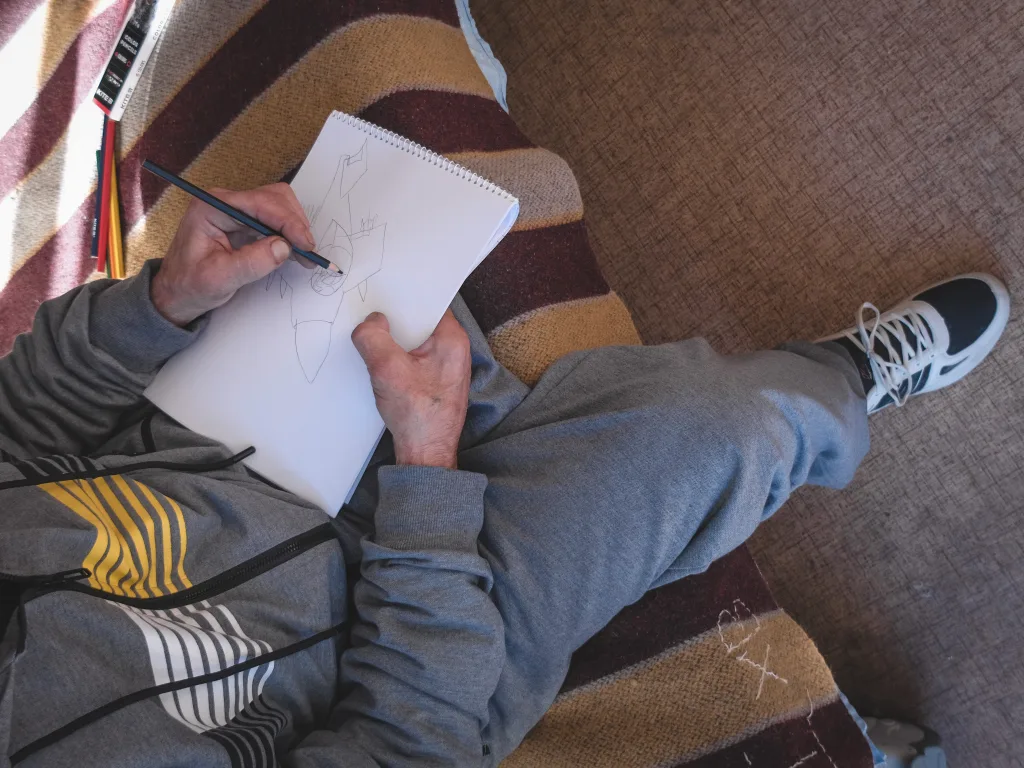
Volodymyr’s story
42-year-old Volodymyr arrived at Cherkasy hospital with injuries to his legs and arms. One of his fingers had to be amputated. He also experienced severe anxiety, sleep disturbances and nightmares. As a guitarist and sound engineer, the amputation of his finger had a profound impact on him. “I used to express everything in my soul through my fingers, but now I can’t play,” Volodymyr says. The team of psychologists at Doctors Without Borders helped him come to terms with his loss. “Psychologists are the people I can tell everything to – they listen to everything about my pain,” he says.
According to the Médecins Sans Frontières mental health team, patients’ opinions and the support of their families and friends play a crucial role in their successful recovery. In addition to providing patients with one-to-one psychological support, the team also conducts group sessions and works with patients’ families.
Through early rehabilitation, Médecins Sans Frontières aims to improve patients’ quality of life, stabilise their emotional state, reduce pain and prevent long-term complications often associated with severe injuries, including the risks of infection and muscle atrophy. Ultimately, this approach aims to restore patient autonomy so that those with severe injuries can take care of themselves in the future.





Read also: The UN: A Mission of Peace and Development
Challenges in implementing rehabilitation services
Despite the obvious advantages of an interdisciplinary approach to rehabilitation care, its implementation in Ukrainian hospitals is difficult because there are currently too few staff with the appropriate qualifications. But this may change in the coming years, says Thomas Marchese, emergency coordinator at Médecins Sans Frontières.
“Although more and more students are now being trained in relevant medical competencies, it will take another three to four years before they start working in all the necessary areas, such as physiotherapy and clinical psychology,” says Marchese.
To bridge the gap between the great needs of people and the limited number of qualified staff, Médecins Sans Frontières proposes to make the best use of available resources and try to reach as many patients as possible. The Médecins Sans Frontières team is working closely with the Ministry of Health sof Ukraine and other partners to make the experience of the interdisciplinary approach to early rehabilitation in Cherkasy possible for more regions. The goal is to reduce the impact of complex war-related trauma on the entire population of Ukraine.
Text: Nadiya Voloboeva
Cover and photos in the text: Yulia Trofimova/MSF, Angelina Schors/MSF
Read also: Moscow Conventions: How Russia Destroys the Principles of International Law